Benefits Realization from Health Tech

Benefits Realization from Health Tech
In the rapidly expanding universe of digital health and other health tech solutions, what is useful and what is not worth the cost remains the question that slows adoption.
It’s a lot easier to say what benefits we’d like to see from digital heath and other health tech than it is to say how benefits happen consistently. User, clinical and financial benefits fall into several categories that usually include improve access, improve treatment specificity and efficacy, improve efficiency including ease of use, reduce cost, increase quality of outcomes, increase personalization of care.
Who wouldn’t want all that? Not only how this may happen in any given case but how we measure our progress to goal to prioritize our resources effectively remains unpredictable.
This suggests an old rubric in health tech that goes something like this:
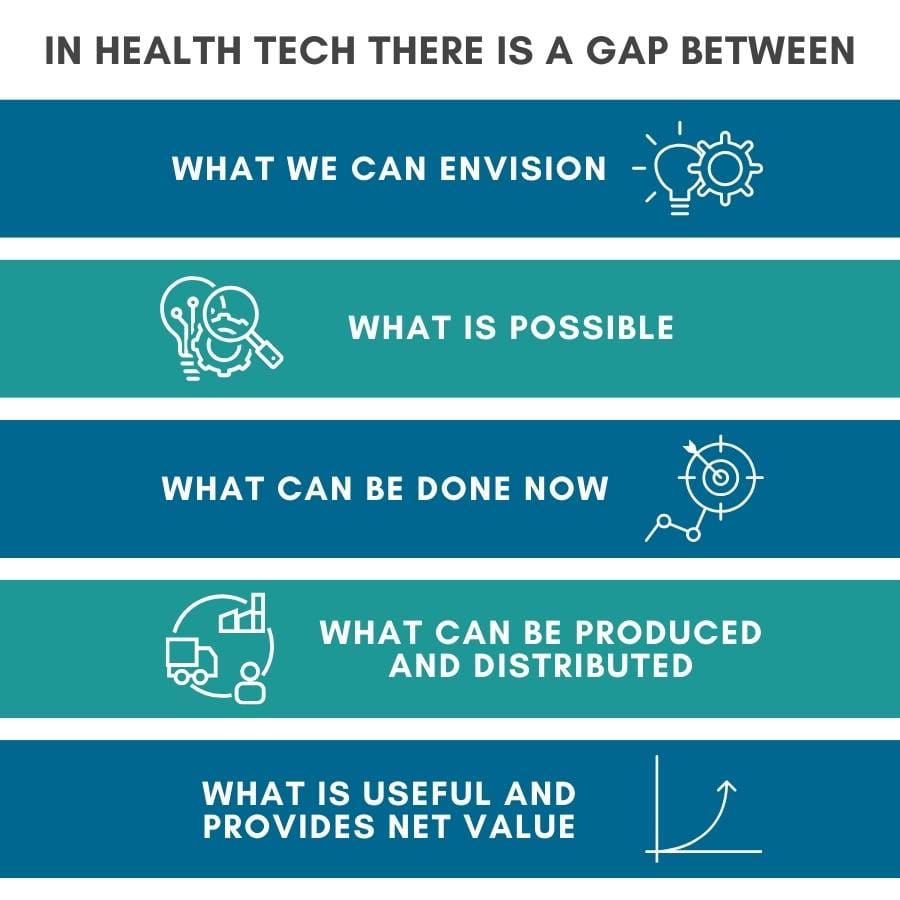
Collapsing these gaps is one level of benefits realization from health tech. At a more operational level benefits or value realization must be tangible for the buyer, the user, and the beneficiary of the technology to result in adoption and acceptance. Value may be difficult to demonstrate when a product is new and innovative. In healthcare it begs the question valuable compared to what?
Going back in time to an opinion piece from JAMA in 2018 authored by David Bates, MD, et.al., the authors suggested policy directions that might standardize how we think about benefits realization from digital health. These included (1) rigorous standardized evaluation methodologies; (2) FDA review of health apps for safety, privacy and false claims; (3) increase support for outcomes research; (4) interoperability between apps and EHRs.
The major issues to be addressed in their view included: Safety, Evidence, Interoperability, and Value demonstration. It is fair to conclude we are still working on it, though we have made some progress in some areas.
In the investment world, Rock Health has suggested using what they call a clinical robustness index calculated based on a company’s total number of FDA filings plus the total number of clinical trials along with peer reviewed publications. Adhering to a rigorous process such as this could be a surrogate or shortcut to determining the likelihood of value creation. Rock Health suggests other criteria be added such as non-clinical outcomes like cost savings, user engagement and peer comparisons.
For users of new health tech, what determines benefits and value realization and thus adoption and acceptance may depend on several considerations. The Productivity Paradox is what happens when a new technology designed to provide improvements in process, productivity, and clinical and financial outcomes fails to do so because the user environment was not prepped for change by process improvement to benefit from the technologic features. Sometimes this is because the technology is flawed and requires iterations of improvement, but more often it is because the organization is unable mange the people, process and workflow changes needed to realize the gains.
These issues reside in the processes, structure, workflow, talent and culture of an organization. In healthcare, the most recent large-scale example is the EHR implementation beginning in 2010. Even when internal capabilities existed in an organization, the first pass implementation often involved automating existing manual processes without managing the needed change. This is called Stage 1 automation wherein inefficient manual processes are memorialized in automated processes. While some benefits accrue, new losses of productivity frequently appear.
Standard work in technology benefits realization involves analytic and process automation that are supportive of user work, that is, realizing productivity gains as well as improved clinical and financial outcomes. Managing the changes to clinical work patterns, tools, and talent to ensure the beneficiary – usually a patient – receives the optimal care at the optimal time remains the goal. The approaches to make this happen have been around through the last 2 or 3 cycles of health tech advances but are apt now.
Driving us forward currently are advancing acceptance of information access and utilization through the FHIR standard and enhanced interoperability. Additionally, machine learning and advances in artificial intelligence with large language model chatbots and applications in automation of analytics and processes may help overcome the productivity paradox for digital health and larger health tech.

