The Decision Bubble
The healthcare product for a hundred years has been a biotechnology-based, information-dependent, personal service. Nothing about chatbot deployment with generative AI will change this definition. In the delivery of care, The Decision Bubble – that set of complex cognitive tasks that highly trained and experienced humans must continue to do—will be enhanced.
The core of medical care delivery, leaving aside the broader opportunities in the meaning of healthcare, is dependent on the process of human decisioning. During the delivery of healthcare, information is required at the point of service.
Decisioning is the active process of maneuvering information, probabilities, likelihoods, and individual values and desires to allow a valid and reproducible decision to be made among alternatives. (Dacso, C., et.al. Project on Decisioning, 2003.)
Making good judgments and decisions about health, whether directed by a clinician or self-directed by individuals, requires access to any information that may be needed. Up until now, this has been more vision than reality.
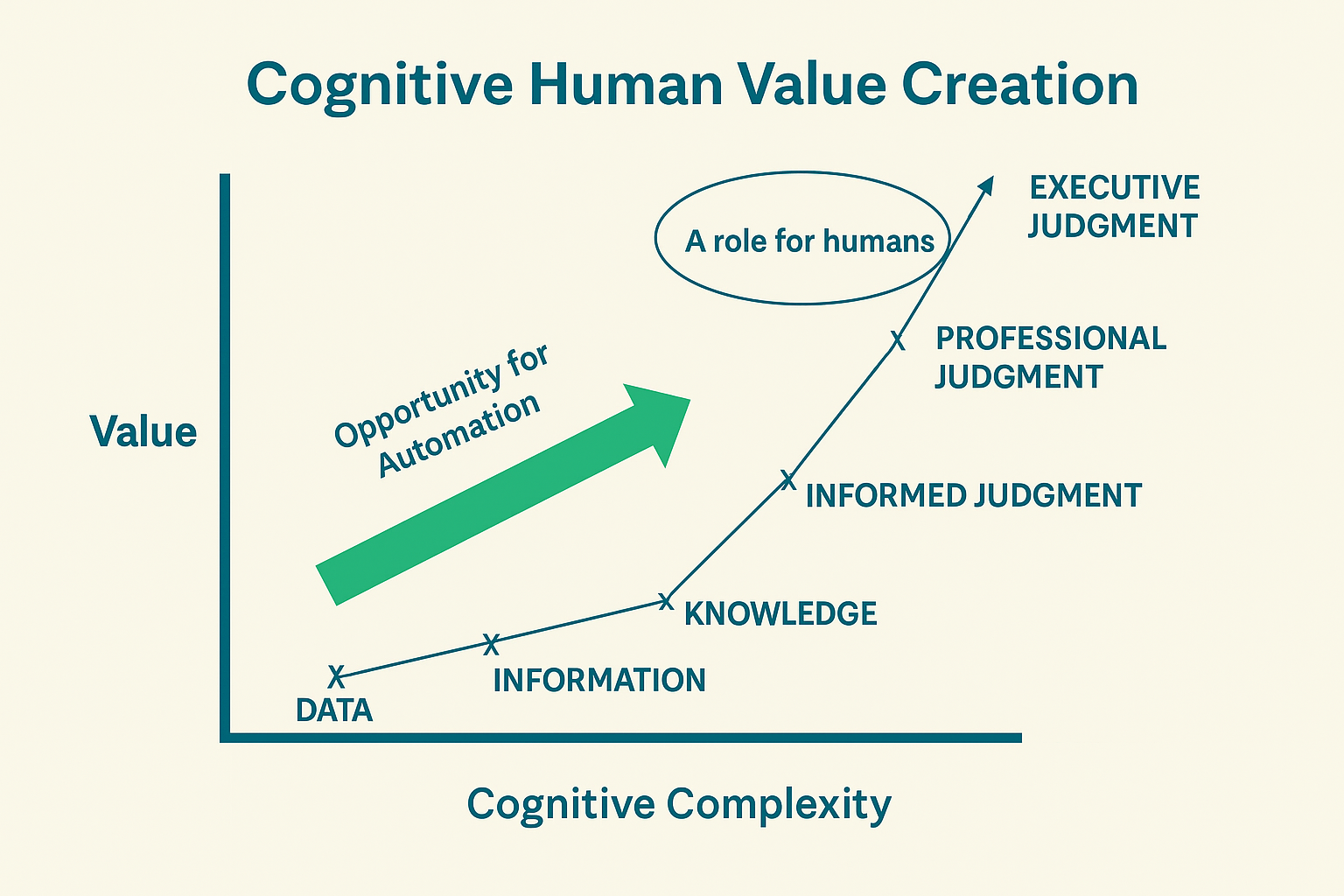
Human Decisioning in Healthcare—Automate clinical and business information flow to facilitate human decision-making.
Despite progress in acquiring data and advances in artificial intelligence and machine learning, humans remain central to decisioning in healthcare. Humans, even with the latest advances in AI, are required to render professional or executive-level judgment. Cognitive complexity relates to the value of decisions. While some steps can be automated, so far, others are not there with the required level of precision and predictability.
Thus, caregivers and physicians must stay in the cognitively complex decision bubble to focus on the vital aspects of clinical decision-making, judgment, and inference, where they provide the most value and where they are uniquely skilled. The flow of information into and out of the Bubble can be automated.
One fallacy of the electronic health record was a design that required the highest skilled and highest paid people to do tasks that did not conform to the complex cognitive tasks where they are primarily needed—diagnosis, decisioning, and prescription. In this way, value was removed from the overall output of the process. Time and effort have been spent in trying to displace the most difficult part of the process, the professional portion, and to degrade the value of professional input to the lowest value-add function, data entry.
The arrival of chatbots and generative artificial intelligence with large language models has made the concept of the Decision Bubble much more likely to occur sooner. There have been many well-described barriers to automating processes and analytics as a flow to the point of care to support diagnosis and prescription as well as the output of assigning tasks and actions.
Already this is beginning to change. For example, early adoption and integration of digital applications in clinical support by chatbots and generative AI include coding, note-taking, prior authorization, care navigation including patient communication, and data synthesis and summarization. Many more should be coming online as we learn to leverage these new technologies. It’s an exciting time, but one where we must be diligent to assure benefits achievement while not creating new problems.